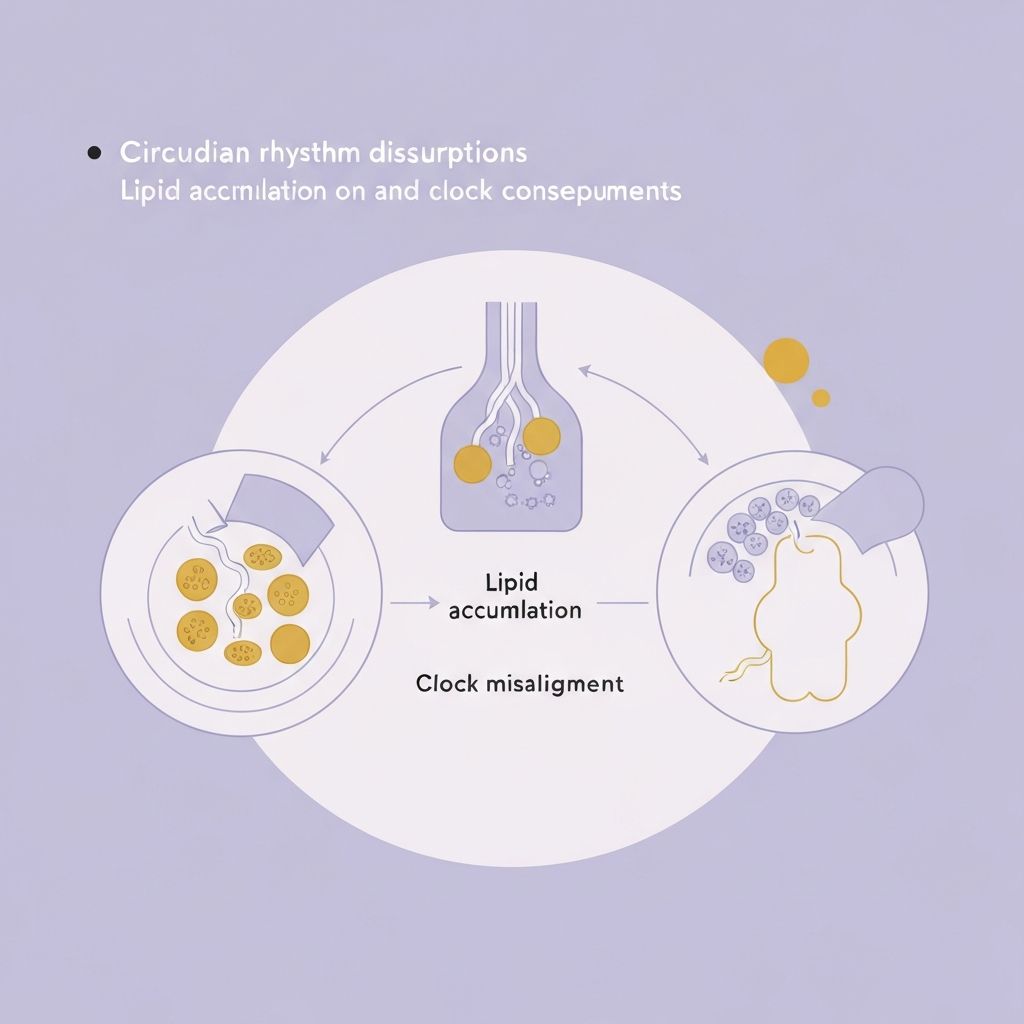
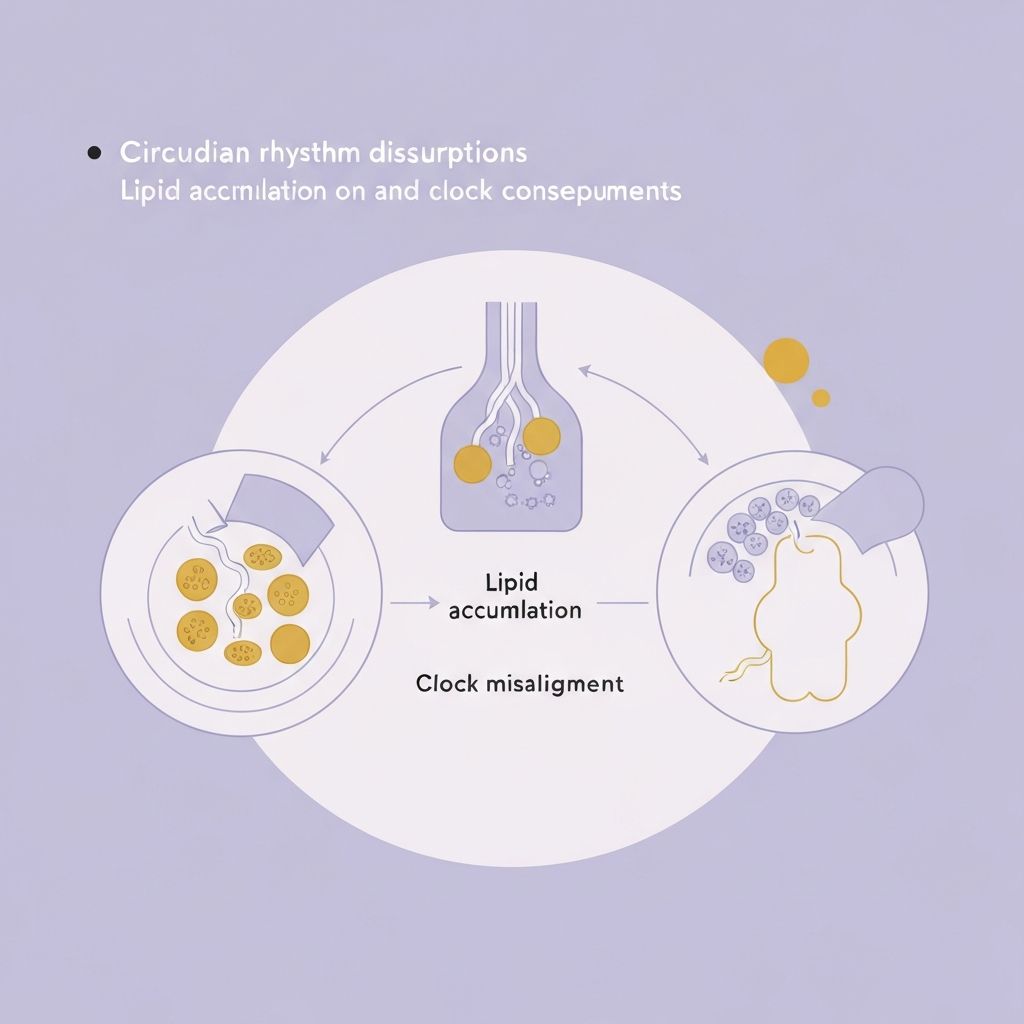
Circadian Rhythm Disruption and Lipid Accumulation
Examining how clock gene dysregulation and circadian misalignment promote visceral adiposity and dyslipidemia.
Clock Gene Expression and Metabolic Regulation
Circadian rhythms are generated by autonomous oscillators present in virtually all cells, driven by core clock genes including BMAL1, CLOCK, PER1, PER2, PER3, CRY1, and CRY2. These genes regulate the expression of thousands of downstream genes controlling metabolism, with approximately 10-15% of the mammalian genome demonstrating circadian rhythmicity. Clock gene expression in metabolic tissues—particularly adipose tissue and liver—directly controls the expression of genes regulating lipogenesis, lipolysis, and cholesterol metabolism.
PPARγ, a critical transcription factor controlling adipogenic gene expression and lipid storage, demonstrates circadian regulation through direct interaction with BMAL1 and CLOCK. Lipoprotein lipase (LPL), the enzyme catalyzing triglyceride hydrolysis and lipid uptake into adipose tissue, exhibits peak activity during the early sleep period in normally entrained individuals. Adiponectin, an adipokine promoting lipid oxidation and insulin sensitivity, shows circadian variation in secretion with peak concentrations during sleep periods.
Circadian Misalignment and Visceral Adipose Tissue Expansion
Circadian misalignment—occurring with shift work, transmeridian travel, and irregular sleep schedules—produces dysynchronization of peripheral clock gene oscillations, resulting in uncoupling of metabolic gene expression from appropriate time-of-day phases. When LPL activity becomes elevated during wakefulness rather than early sleep, excessive lipid uptake occurs in adipose tissue during periods of active metabolism and elevated lipolysis, promoting net lipid storage. Similarly, dysregulated PPARγ expression leads to inappropriate adipogenic gene transcription and increased adipocyte lipid storage capacity.
Studies examining shift workers demonstrate selective expansion of visceral adipose tissue compared to subcutaneous adipose tissue, a phenomenon reflecting the particular metabolic sensitivity of visceral adipocytes to circadian disruption. This visceral adiposity expansion carries particular metabolic significance because visceral adipose tissue exhibits elevated inflammatory cytokine production, enhanced lipolytic responsiveness to catecholamines, and greater metabolic activation of glucocorticoid hormones compared to subcutaneous adipose tissue.
Clock Gene-Dependent Hepatic Lipid Metabolism
The liver exhibits particularly prominent clock gene expression, with circadian oscillation of genes controlling cholesterol synthesis, bile acid production, and triglyceride metabolism. SREBP1c (sterol regulatory element binding protein 1c), the master transcription factor controlling de novo lipogenesis, demonstrates circadian regulation with peak expression during early sleep periods in normally entrained individuals. Circadian misalignment elevates hepatic SREBP1c expression during wakefulness, promoting fatty acid synthesis during periods when fatty acid oxidation is normally elevated, creating conditions for hepatic triglyceride accumulation.
Clock gene dysregulation in liver also impairs the hepatic lipid export pathway through dysregulation of APOB (apolipoprotein B) expression. The combination of elevated hepatic lipogenesis and impaired hepatic lipid export produces non-alcoholic fatty liver disease (NAFLD) development in circadian-misaligned populations. Experimental studies demonstrating circadian misalignment through scheduled feeding during the sleep period in rodents produce rapid development of fatty liver and hepatic insulin resistance.
Circadian Dysfunction of Adipose Tissue Lipolysis
Adipose tissue lipolysis demonstrates marked circadian variation, with highest hormone-sensitive lipase (HSL) activity during wakefulness and lowest activity during sleep in normally entrained individuals. This pattern allows preferential lipid mobilization during active periods when mobilized fatty acids can be oxidized for energy, while restricting lipolysis during sleep when oxidative capacity is reduced. Circadian misalignment disrupts this coordinated timing, allowing lipolysis to proceed during sleep periods when oxidative capacity is inadequate, promoting re-esterification of liberated fatty acids and net lipid storage.
The dysregulation of adipose tissue clock genes in circadian-misaligned individuals reduces the normal circadian amplitude of HSL activity, resulting in both elevated basal lipolysis during sleep (when it should be suppressed) and potentially reduced peak lipolysis during wakefulness. The net effect depends on the specific pattern of misalignment but generally results in reduced net lipid oxidation and increased net lipid storage compared to circadian-aligned conditions.
Inflammatory Cytokine Production and Dysmetabolism
Circadian misalignment elevates systemic production of pro-inflammatory cytokines including TNF-α, IL-6, and IL-1β. Immune cells, including macrophages and T cells, exhibit circadian variation in inflammatory cytokine production, with peak production typically occurring during the sleep period (at least in normally entrained individuals). Circadian misalignment uncouples immune cell activation from appropriate timing, resulting in elevated inflammatory cytokine production at inappropriate times of day.
Elevated TNF-α and IL-6 directly impair insulin signaling and promote preferential visceral adipose tissue accumulation through TNF-α-mediated effects on adipocyte differentiation and apoptosis. Chronic elevated IL-6 production impairs hepatic insulin clearance and promotes hepatic lipogenesis through activation of SREBP1c. The inflammation accompanying circadian misalignment may represent a key mechanism linking circadian disruption to obesity and metabolic syndrome development.
Melatonin Dysregulation and Lipid Metabolism Effects
Melatonin, a circadian hormone produced by the pineal gland with peak secretion during nocturnal hours in normally entrained individuals, exerts direct inhibitory effects on adipogenesis and promotes lipid oxidation. Melatonin acts through nuclear melatonin receptors to suppress SREBP1c expression and reduce hepatic lipogenesis. Additionally, melatonin scavenges reactive oxygen species (ROS), reducing oxidative stress-induced impairment of mitochondrial lipid oxidation capacity.
Circadian misalignment and irregular sleep-wake cycles dysregulate melatonin secretion, reducing peak melatonin concentrations and producing melatonin secretion at inappropriate times of day. This melatonin dysregulation removes important lipogenic suppression and antioxidant defense, contributing to increased hepatic lipogenesis and reduced lipid oxidation. Experimental melatonin supplementation in circadian-misaligned populations partially reverses metabolic dysregulation, supporting a mechanistic role for melatonin dysregulation in circadian disruption-induced metabolic disease.
Limitations and Context: This article presents information on circadian rhythm biology and lipid metabolism regulation. Individual responses to circadian disruption vary based on genetic factors, age, and baseline metabolic status. This content is for educational purposes only and does not constitute medical advice or recommendations for circadian rhythm management.
Read the detailed physiological explanation
Explore additional articles on sleep stages, hormonal regulation, and longitudinal research evidence on sleep and metabolic health outcomes.
Return to blog overview